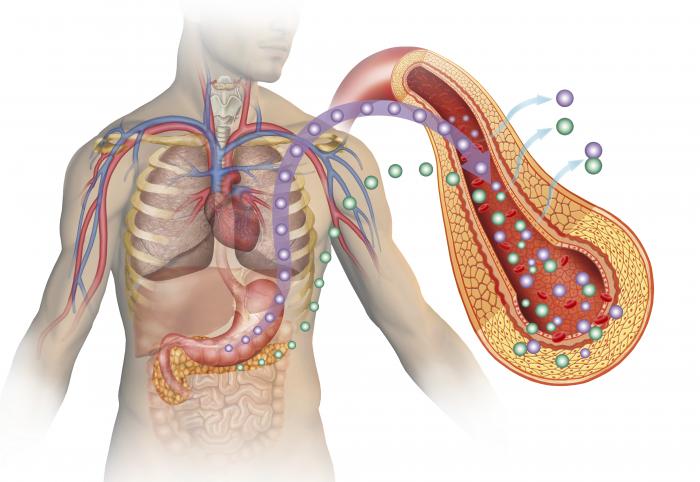
Recently discovered biomarkers may provide valuable new approaches to monitoring immunosuppressive drug therapy in organ transplant recipients–with the potential for individualized therapy to reduce organ rejection and minimize side effects, according to a special article in the April issue of Therapeutic Drug Monitoring, official journal of the International Association of Therapeutic Drug Monitoring and Clinical Toxicology. The journal is published by Wolters Kluwer.
“Biomarkers should help to tailor immunosuppressive therapy to the needs of the individual patient,” according to the review by an international Expert Committee. The initial “Barcelona Consensus Statement” includes a preliminary set of recommended tests for use in biomarker-based immunosuppressive drug management after organ transplantation. The lead author is Mercè Brunet, PhD, of Hospital Clinico de Barcelona.